Dry Eye Therapy: Restoring Healthy Tears
Thank you for choosing Eyecare Medical Group’s Dry Eye & Aesthetics Center for your dry eye care. We look forward to working with you to create a customized treatment plan to relieve your symptoms. This page provides general information about dry eye disease and how we can modify our environment and lifestyle to support healthy tears and minimize dry eye symptoms.
About Dry Eye Disease:
Dry eye disease is one of the most common conditions that affect the eyes. It is estimated that 50 million Americans suffer from dry eye disease and it is becoming more common as we live longer and our environment becomes more conducive to dryness. While dry eyes may sound simple, it is a complex and often poorly understood condition.
“Dry eye disease” is an umbrella term that includes many conditions that result in an unstable tear film that can’t adequately and consistently protect, nourish and hydrate the surface of the eye. It is a chronic, often progressive, condition that affects vision, the comfort of the eyes and, ultimately, quality of life. Common names used for dry eye disease include:
- Keratitis sicca
- Keratoconjunctivitis sicca
- Ocular surface disease
- Lipid deficiency
- Dysfunctional tear film
- Aqueous deficiency syndrome
At best, dry eyes are a nuisance and, at worse, can cause significant discomfort and poor vision. People can experience dry eye symptoms in many different ways and symptoms do not always correlate with severity. Interestingly, ~40% of patients with dry eye findings report no symptoms.
Until recently, we have largely overlooked the importance of healthy tears and the impact of dry eye disease. This is a complex, inflammatory condition with various presentations and causes. Like many other chronic conditions, changes can occur over many years, and worsen at any time, before significant symptoms are experienced. Advancements in research and technology have to lead to improved treatments and better relief of symptoms. Effective therapy is aimed at minimizing inflammation and supporting healthy tears.
We now know the best time to address dry eye disease is early in the process before significant changes occur. There are many lifestyles and environmental modifications that can be made to support healthy tears and minimize symptoms. Successful dry eye therapy starts with understanding what is happening and what we can do to help.
Common symptoms of dry eyes include:
- Burning or stinging
- red eyes
- Grittiness or foreign body sensation
- light sensitivity
- fluctuating vision with blinking
- poor reading vision
- sensitivity to cold and/or windy environments
- pain or soreness of the eyes
- itchy eyelids
- decreased contact lens tolerance
- sticky eyes
- watering eyes
- tired eyes
The Importance of Healthy Tears
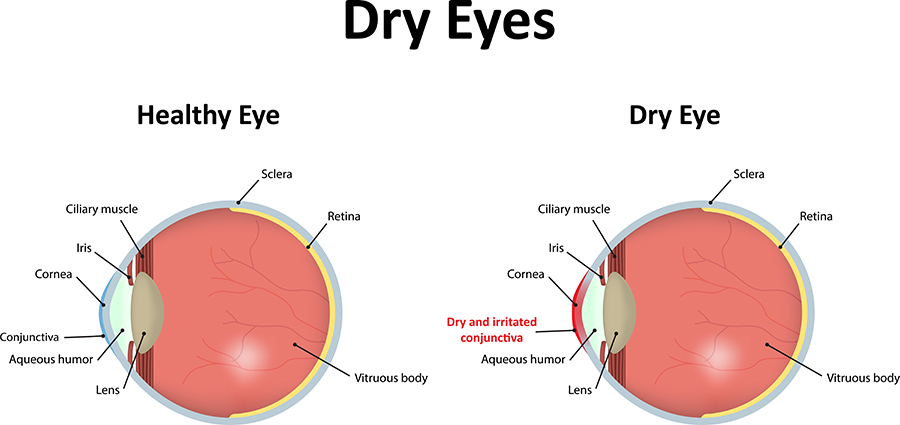
Dry eyes happen when the tear film fails and the eye is over-exposed to the environment, causing discomfort and inflammation. The surface of the eye (the cornea) is a mucous membrane and must stay hydrated to be healthy and comfortable. If someone does not produce enough tears, does not produce quality tears, and/or cannot evenly spread tears over the eyes, he/she will be at risk for developing dry eye disease.
When we blink, our eyelids close in a squeegee-like manner from the outer to inner corners of our eyes, clearing old tears into the tear ducts and spreading fresh tears uniformly across the eye.
The tear film serves multiple functions:
- Maintains hydration of the surface of the eye.
- Clears debris, allergens and other particles to avoid irritation and damage to the eye.
- It provides a strong immune system to protect the eye from infection.
- It provides nutrients to the surface of the eye, the most metabolically active and fastest healing tissue of our body.
- It provides a smooth refractive surface for clear vision, focusing ~80% of light as it enters the eye.
- The tear film is a remarkably complex structure comprised of essential fatty oils, proteins, vitamins, electrolytes, antibodies, and water suspended in a delicate balance.
The tear film is made of three unique, interactive layers:
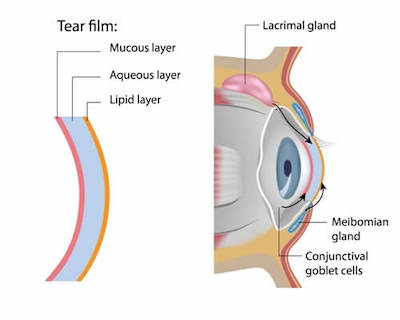
The lipid (“meibum”) layer is the outermost layer of the tear film. It thickens the tears, creates a smooth surface for light to focus through and slows the evaporation of tears. This layer comes from the meibomian glands located within the eyelids. When our eyelids come to a close during a full blink, muscles within the eyelids squeeze oil over the tears.
The aqueous layer is the watering middle layer of the tear film. It makes up most of what we see as tears and washes away particles that do not belong in the eye. This layer comes from the lacrimal gland, located behind the upper eyelid.
The mucin layer is the inner layer of the tear film. This creates the base to help evenly spread the tears over the entire eye’s surface. Without mucin, tears would not stick to or evenly spread over the eye. Mucin is made from goblets cells within the conjunctiva.
Our tears are made and regulated by the Lacrimal Functional Unit (LFU), a fully integrated system involving all structures and neural pathways active in tear production. In a healthy functioning tear system, the eyes are constantly making balanced tears that alter composition based on changes in the environment. Dry eyes occur when this system dysfunctions and the tears becoming increasingly imbalanced and unstable. Anything that affects the body’s ability to make enough tears, quality tears and/or spread the tears evenly across the eyes increases the risk of dry eye disease. If the tears are kept in a chronic state of imbalance, an inflammatory cycle can result and the health of the eyes and quality of vision can suffer.
Sub-Types of Dry Eyes Disease
Historically, dry eye disease has been classified as one of two types: 1) aqueous deficiency, primarily due to low tear production, and 2) lipid deficiency, primarily due to meibomian gland dysfunction and/or blepharitis. Because the tears are in constant contact with the lid margins, the health of the tears and the health of the eyelids directly impact one another. We now know the majority of dry eye cases are a mixture of lipid deficiency and aqueous deficiency and may also involve mechanical factors.
Lipid Deficiency aka Meibomian Gland Dysfunction:
Lipid deficiency, meaning too little oil in tears, causes rapid tear evaporation and is a very common cause of dry eye disease. Poor oil production results when the meibomian glands of the eyelids do not function properly. This can happen for many reasons, including the use of certain medications, blepharitis (below), increased inflammation within the body and poor blinking. Treatment is aimed at improving oil quality and movement into the tears.
Blepharitis:
Inflammation along the eyelid margin is common across the general population and results in lid irritation, redness, and itching. It is more common in people with fair complexions or skin conditions such as rosacea, eczema, and psoriasis. Cosmetic and hygiene habits can greatly impact blepharitis. Treatment is aimed at properly cleaning the eyelids and modifying habits to minimize inflammation.
Aqueous Deficiency:
Low tear production from the lacrimal gland, or aqueous deficiency, is mostly associated with certain medications, increased age, dehydration, and autoimmune conditions. Treatment is aimed at increasing tear production through prescription eye drops, increasing hydration and modifying the environment to increase humidity.
Mechanical Factors:
Anything that alters proper blink function can affect tear stability and result in dryness. Prior eyelid surgeries, Bells Palsy, incomplete lid closure, incomplete and/or infrequent blinks, increased screen time and eyelid laxity can all impact blink function. Treatment often includes improving blink habits, overnight lubrication, moisture goggles, modifying the environment and surgical lid procedures, if needed.
Common Risk Factors Associated with Dry Eyes
Environmental and Lifestyle Modifications to Improve Dry Eyes Symptoms
Nutrition and Dry Eyes
Healthy eyes belong to healthy bodies. Living a healthy lifestyle, staying active and eating a well balanced, wholesome diet is important to keeping your eyes healthy. A diet that minimizes inflammation and provides essential nutrients is important for dry eyes.
If you feel your diet may be lacking in nutrients, you can consider taking supplements:
- Daily multivitamin
- Lutein + zeaxanthin
- carotenoid pigments important for general eye health
Omega-3/6/9 Supplements:
- 1,000-2,000mg Omega-3/6/9 (DHA + EPA + GLA) every morning with a full glass of water and high-fat breakfast (avocado, eggs, peanut butter smoothie, etc.) to maximize absorption. If unable to tolerate full dose at once, split doses breakfast/dinner.
- can double dose for 15-30 days when starting supplements or every 6-12 months as needed to control symptoms
- vegetarian options:
- 1-2 tablespoons of cold-pressed flaxseed oil (store in fridge)
- 1-2 tablespoons of fresh ground flaxseeds added to food (hot or cold cereal, yogurt, smoothies, juice, etc.)
- Omega-3 supplements can contribute to the thinning of the blood. Consult your doctor before starting supplements if you are pregnant or taking prescription blood thinners such as Lasix, Coumadin, Xarelto or daily aspirin.
- consider taking a lipase enzyme if poorly functioning or missing gallbladder.
The Importance of Blinking
The vast majority of us do not blink frequently or fully enough throughout our day. We blink half the normal rate when concentrating (eg. reading or driving), a fifth of the normal rate when using electronic devices (eg. computers, TVs and smartphones) and many of us resort to quick, rapid blinks under these conditions. This creates a tear film that is not fully replenished or evenly spread across the eye, often worsening dry eye symptoms. There are also a number of medications and conditions that can contribute to incomplete and/or infrequent blinking.
During a full blink, the upper and lower eyelids come together in a squeegee-like manner, clearing tears and creating fresh tears.
When the lids come to a complete close, muscles within the eyelids squeeze the meibomian glands and release oil into the tears while the eyelids subtly rub back and forth and clean the lashes. When the lids open, the tear film is spread uniformly across the eye.
It is important to take frequent breaks when concentrating, especially when working within your arms reach or on electronic devices, to avoid dryness and eyestrain:
• Vision Hygiene 20/20/20 • every 20mins, look 20+ feet away for 20+ seconds and take 20 slow, long blinks
“Conscious blinking” is as simple as taking a few slow, long, deliberate blinks and holding mid-blink for 2 seconds. Try to connect this with things that occur frequently throughout your day, such as between emails, phone calls, meals or breaks. Take a few long blinks after warm compresses and lid hygiene, too.
- Close to teach the lids to touch
- Pause for a count of 2 to reinforce the lids touching
- Open for a count of 2 to complete the blinking sequence
Computer Programs to Remind Blinking Breaks:
PC compatible:
FREE
- www.workrave.org | www.trisunsoft.com/pc-work-break
- www.eyeleo.com | www.regularbreaks.com
FEE-BASED
- www.paratec.com | www.eyeprotectorpro.com
iOS (Apple) compatible:
FREE
- www.regularbreaks.com, Timeout (Mac only in App store)
Lid Hygiene
Regular cleaning of the lid margin is important. Without regular cleaning of lids and lashes, a buildup of dead skin cells, oils, make-up, and debris collects along the lids and sticks to the base of the lashes. This buildup increases inflammation along with the lids and blocks oil glands. The goal of lid cleaning is to clean the lid margin of all debris without stripping the good oils and flora, open oil glands at the base of lashes and limit overall inflammation of lids and tears.
We recommend doing whatever hygiene routine is most convenient and comfortable for you. Some people prefer to use foaming cleansers in the shower and lid wipes, otherwise. Some choose to alternate okra-based and tea tree-based products. And some choose to use lid spray after lid cleansers every time, every few times or not at all while others choose to use only lid spray with no other cleansers. There is no right or wrong way to clean the lids, just have some sort of routine in place. And, just like dental hygiene, anything is better than nothing.
Artificial Tears
Artificial tears are helpful in dry eye management, but they do not improve the quality of the natural tears.

Benefits of artificial tears:
- Soothes and hydrates the surface of the eye
- Stabilizes and balances tear film
- Aids in spreading tears across the eye
- Rinses toxins, irritants, and debris from eye
- Reduces blink friction between eyelid and surface of the eye
Not all artificial tears are made the same. We will provide you with a list of recommended options. It is important to choose quality drops with gentle preservatives. Avoid generic brands, as they often use harsh preservatives such as benzalkonium chloride (BAK) which can worsen symptoms.
Brands Include:
- Refresh
- Systane
- Oasis
- Blink
- Genteal
- TheraTears
- Soothe
- Retaine
All recommended drops are good options, but some may be more soothing than others. Use whichever feels the best for you.
Tips & Tricks About Artificial Tears:
- Use tears before activities that bother eyes, such as computer use, reading, driving, outdoor activities, etc.
- Store drops in the fridge to be cooling and extra soothing, if needed.
- Artificial tears are not the same as “redness relievers” or “itch relievers”, which have additional medicines that are not always helpful.
- Don’t share eye drops with other people.
- Do not touch dropper tip to eye, eyelashes or eyelid.
- Remove contact lenses before using any eye drops not intended for use with contacts.
- If you are taking more than one type of eye drops at the same time, wait 3-5 minutes between drops.
PRESERVED TEARS
- multi-use bottle
- do not use over 4 times/day
- chose drops with gentle preservatives
- throw away 2-3mths
PRESERVATIVE-FREE TEARS
- ok to use 4x/day, not to exceed every 1-2 hours
- single-use vials must be thrown away at end of day
- use preservative-free vials if you have severe dryness or sensitive skin or eyes
In general, the use of redness relievers is discouraged. When used frequently, “rebound redness” occurs, meaning the eyes will be red unless you use the drop. Additionally, these drops tend to use harsh preservatives. They should be used very sparingly, if at all.





